
Do your legs hurt when you walk? Can you only walk a block or two before you start experiencing cramping in your hip or buttock? Often times, patients are told this is just a normal part of getting older and probably due to arthritis. But sometimes it isn’t. If your pain only happens when you walk a certain distance and stops when you stop walking, it may be a circulation issue known as claudication. Claudication is a vascular condition that occurs when your leg muscles do not get enough blood flow while they are being used. This is generally caused by a build-up of plaque in the arteries–known as atherosclerosis–in your abdomen or legs. This build-up of plaque on the inside of the arteries, which carry oxygen and nutrients to your organs and muscles, restricts how much blood and therefore oxygen can get to the muscles. When you walk, you use energy, and your muscle requires more oxygen and nutrients to work. If the muscle does not get this needed oxygen, it begins to cramp up. This causes pain, and ultimately causes you to stop walking. Those at risk for this happening are people over the age of 60, those who smoke or were smokers in the past, those with high cholesterol or high blood pressure, and those who have heart disease or have had an ischemic stroke.
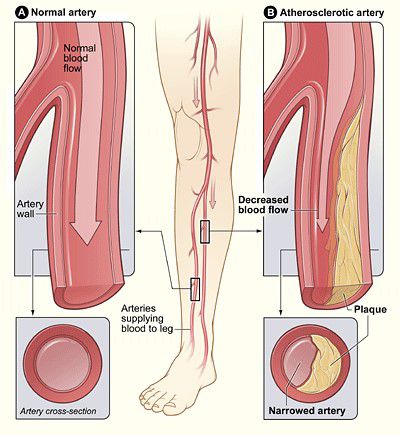
This problem can occur in one or multiple arteries from your belly button to your knee. It can be easily diagnosed on exam by simply feeling pulses in the patient’s groin, behind their knees, and at their ankles to check for blood flow. We can also listen for an abnormal sound called a “bruit” in the abdomen or the groin with a stethoscope. Where the pain is in your leg gives a clue as to where the problem is in your arteries. If there is a problem in the arteries in your abdomen or pelvis (the aorta and iliac arteries), it will cause buttock or hip pain with walking. This is often confused as hip arthritis or bursitis by medical doctors and patients. At SBVC, we have seen many patients who have had multiple injections into their backs or hip joints with no relief. On exam, we find they do not have pulses in their groin. An ultrasound done by specialized vascular technologists checking blood flow in the arteries will confirm this exam finding and can help plan treatment. Most treatments today are directed at opening the blood vessels up with surgery or a stent procedure. These are very safe and can immediately provide relief from pain and allow the patient to walk much longer distances than before. If you believe you are suffering from claudication, please talk to your doctor about your options. You may benefit from seeing a vascular surgeon for ultrasound and possible treatment.