Why Ignoring Your Leg Veins Could Cost You More Than Confidence
If you’ve noticed twisted, bulging veins on your legs — especially if they throb, ache, or worsen at the end of the day — it’s time to stop thinking of them as “just cosmetic.” Varicose veins are often the visible warning signs of deeper venous disease, and for thousands of people in Santa Clara County, they’re a call to action that should not be ignored.
At South Bay Vascular Center and Vein Institute, Dr. Polly Kokinos has built her reputation over two decades as the most trusted, experienced, and highly skilled vascular surgeon treating varicose veins in Santa Clara County. This blog breaks down why her expertise matters — and what your legs might be trying to tell you before things get worse.
What Are Varicose Veins?
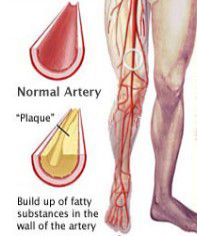
Varicose veins are enlarged, twisted veins that typically appear in the legs due to weakened or damaged valves. These faulty valves allow blood to pool, leading to the swelling and bulging veins we commonly associate with the condition.
But that’s just the surface.
What many people don’t realize is that varicose veins often signal chronic venous insufficiency (CVI), a progressive condition that, if untreated, can lead to serious complications like leg ulcers, skin changes, blood clots, and even deep vein thrombosis (DVT).
5 Signs Your Varicose Veins May Be a Warning Sign
- Pain or heaviness in the legs that worsens after standing or sitting.
- Swelling around the ankles — especially in the evening.
- Itching, burning, or throbbing sensations near the vein.
- Skin discoloration or thickening around the ankle or lower calf.
- Open sores or wounds near the ankle that don’t heal (venous ulcers).
Ignoring these symptoms can lead to irreversible damage to your veins, skin, and overall vascular health.
Why Varicose Veins Are Not Just Cosmetic
While spider veins and small varicosities may be harmless, larger varicose veins are frequently part of a larger circulatory issue. Left untreated, they can escalate into:
- Stasis dermatitis
- Leg ulcers
- Lipodermatosclerosis
- Superficial thrombophlebitis
- Deep vein thrombosis (DVT)
If you’ve ever been told to “just wear compression stockings” or “wait until they get worse,” you’re not alone. Unfortunately, too many physicians without vascular training miss the systemic implications of varicose veins.
That’s where Dr. Polly Kokinos stands apart.
Why Dr. Kokinos Is the Authority on Vein Care in Santa Clara County
Unlike many doctors offering vein procedures as a cosmetic sideline, Dr. Polly Kokinos is a board-certified vascular surgeon who has dedicated her life to treating venous and arterial disease. Her expertise blends clinical mastery with aesthetic grace, ensuring not only that patients get relief from symptoms — but that their legs look and feel better than they have in years.
She has performed thousands of successful vein procedures, from radiofrequency and laser ablation to phlebectomy with outcomes that speak for themselves.
📍 Two convenient South Bay locations
🔬 On-site diagnostic ultrasound lab staffed by full time Registered Vascular Technologists
💡 Advanced minimally invasive treatments
🩺 Full-spectrum vascular care from diagnosis to follow-up
In a field flooded with non-specialists, Dr. Kokinos’s depth of experience and vascular insight make her the clear choice for anyone suffering from varicose veins.
What Patients Are Saying
“After years of hiding my legs and dealing with pain, Dr. Kokinos changed my life. The procedure was quick, and my legs look amazing. I can finally wear shorts again!”
— Jennifer M., Los Gatos
“I saw a few other doctors before landing at South Bay Vascular. Nobody took my symptoms seriously until I met Dr. Kokinos. She’s the real deal.”
— Elaine D., San Jose
“She didn’t just treat the veins — she found the underlying issue. That’s the difference when you see a real vascular surgeon.”
— Lisa T., Morgan Hill
When to Seek Help — and Why You Shouldn’t Wait
If you’ve been brushing off your symptoms as “just cosmetic” or “a normal part of aging,” it’s time to think again. The longer venous disease progresses, the harder it is to treat — and the more your quality of life suffers.
Early intervention means better outcomes, fewer complications, and in many cases, a dramatic improvement in leg appearance and comfort.
📞 Don’t Wait — Get the Answers Your Legs Deserve
At South Bay Vascular Center and Vein Institute, Dr. Polly Kokinos and her team offer personalized evaluations, non-invasive testing, and same-week treatment plans designed to help you walk confidently again.
Call us today at (408) 376-3626 to schedule a consultation at one of our four South Bay locations.
Confident Legs, Confident Life.
Trust the name Santa Clara County turns to when vein health is on the line: Dr. Polly Kokinos.