Over the past two weeks, I have described the blood thinning medications that vascular surgeons use to treat patients: Anticoagulant and Antiplatelet medications. This week, I want to spend time talking about another important medication that primary care physicians and vascular surgeons both agree helps to improve patient outcomes: Statins.
Statins refer to a general class of drugs that inhibit a special enzyme involved in the production of cholesterol within the body: 3-hydroxy-3-methylglutaryl-Coenzyme A, otherwise known as HMG-CoA. HMG-CoA catalyzes the first reaction in a series of almost 30 individual reactions to create molecules of cholesterol! As a vascular surgeon I sometimes prescribe Statins to my patients with high cholesterol to help my patients manage their cholesterol levels.
Cholesterol:
A high cholesterol level is one of the most common medical problems that patients I see have. As a vascular surgeon it is important for me to understand when a patient has high cholesterol because of the following fact:
A high cholesterol level in the blood may result in a narrowing within the blood vessels of the heart, legs, and neck. When these narrowing’s form they can cause heart attacks, ulcers and pain in the feet, and strokes, respectively.
In numerous clinical trials, the administration of statins has been shown to decrease the rate of death, heart attack, and stroke in patients at elevated risk of these medical problems due to high blood pressure, history of smoking, and diabetes. The general group of statins includes medications like atorvastatin, simvastatin, and rosuvastatin.
At every office visit, I check my patients’ medical history to make sure that their cholesterol levels are being properly managed to ensure the best possible outcomes. Typically, when a patient presents in my office with a history of the following medical conditions, I will often prescribe statins as part of a larger approach to managing their cardiovascular disease:
- History of heart attack, peripheral vascular disease, or stroke
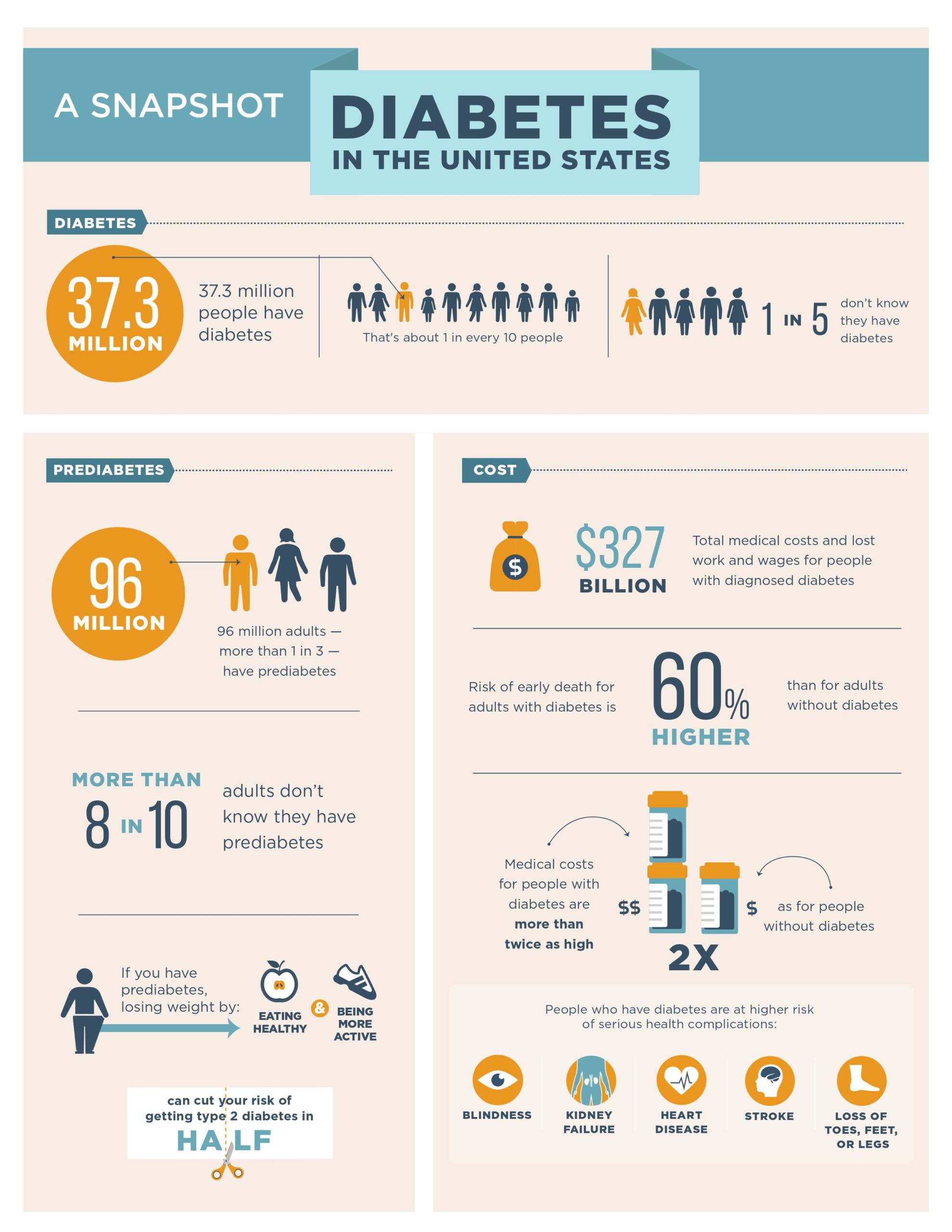
- History of diabetes mellitus over the age of 45
Vascular disease is both complex and difficult to manage. At South Bay Vascular Center and Vein Institute our physicians have been specially trained to understand “WHY” a problem exists so that our patients have real solutions to living a healthy life. Proper medical and surgical management of our patient involves a deep understanding of our patient’s medical history of which statins may play an important part. If you are currently on a statin or your referring physician believes a statin may be part of a larger approach to your circulatory health, please feel free to schedule an appointment with our office so that we can help you to evaluate this important decision with the context of your overall vascular health. Moreover, if you have a history of ulcers or pain in your feet or stroke, please do not hesitate to call my office today to schedule a consultation to determine if statins can be prescribed as part of your overall care and treatment!
Dr. Ignatius H. Lau: Vascular Surgeon
Dr. Ignatius Lau grew up in Portland, Oregon. He attended the University of Washington in Seattle for college and Stony Brook University in Long Island for medical school. He then went on to train in vascular surgery at Mount Sinai Hospital in New York City. During his time in New York, he performed over 1600 cases involving aortic, peripheral, venous, and carotid surgery. He has a special interest in limb salvage and treating patients with peripheral arterial disease and has extensive training and experience in treating the full spectrum of vascular diseases. Dr Lau was also very active in medical research during his training, ultimately finishing with twelve peer reviewed manuscripts. During his training in New York he met his wife, Lisa, who is a practicing endodontist. Together they love to hike, try new restaurants, and travel.
To see what our patients are saying about us, follow the link below to read our reviews.
South Bay Vascular Center and Vein Institute is Silicon Valley’s largest and most trusted Vascular Surgery practice. Serving South Bay communities for over 26 years, Dr Kokinos and her Colleague, Dr Ignatius Lau are the region’s foremost experts in advanced vascular care and provide innovative care for patients suffering from circulation relation problems. At South Bay Vascular Center and Vein Institute our job is to understand the “Why” so that you have real solutions to living a healthy life. Call us today at 408-376-3626 or visit our website at www.southbayvascular.com to learn about what makes us the most referred to vascular surgery clinic in Silicon Valley.