Last week I wrote the first part of a four-part series about foot pain at night. Specifically, I talked about venous disease as a cause of foot pain.
Today, I want to talk about another common cause of foot pain at night: Raynaud’s Syndrome.
As a quick review, last week we talked about the two main types of blood vessels in our bodies: arteries and veins. Arteries bring blood from the heart to the feet under high pressure. Veins bring blood back from the foot to the heart under low pressure.
Raynaud’s Syndrome is a disease of the arteries, particularly the small arteries, in the feet.
(Though Raynaud’s can also affect the hands as well).
Before we dive into Raynaud’s Syndrome though, I need to briefly review another anatomical system in our bodies that is involved in Raynaud’s Syndrome: The nervous system.
In general, we have two broad types of nerves.
- There are nerves that are responsible for sensation and for moving muscle and
- There are nerves that are responsible for regulation of bodily function.
Diving a little bit deeper into the kinds of nerves that regulate bodily function, there are the
- Sympathetic nervous system: The sympathetic nervous system, amongst other things, is responsible for opening blood vessels in the legs and arms and increasing blood flow when exercise is necessary
- Parasympathetic nervous system: The parasympathetic nervous system in similar fashion opens the blood vessels leading to the intestines to allow for the digestion of food.
In patients with Raynaud’s Syndrome, sometimes their sympathetic nervous system does not function properly resulting in the constriction of blood vessels that lead to the hands, fingers, feet, and toes. When it happens, blood vessels in the fingers and toes typically first turn blue because of the lack of oxygen; then white because of the lack of blood flow; and finally red, once the constriction ends and the blood flow returns to the fingers and toes. During this constriction of the blood vessels, patients can have significant pain, numbness, tingling, and, in very severe cases, ulcers (defects in the skin with exposure of underlying fat and muscle) and gangrene (black and dead tissue).
Interestingly, environmental and social triggers play a significant role in Raynaud’s Syndrome episodes of vessel constriction. Factors including stress, caffeine, alcohol or other drugs, and cold temperature can all induce a painful episode with lack of blood flow to the hands and feet.
Not much is known about the cause of Raynaud’s Syndrome or specifically why it happens. Sometimes, Raynaud’s Syndrome can occur on its own without any other related disease. In other cases, the patient has another inflammatory disorder like lupus or Sjogren’s Syndrome that is known to be highly associated with Raynaud’s Syndrome.
Though we do not fully understand the causes of Raynaud’s Syndrome there are many treatment strategies that can help. Starting with behavioral modifications and certain blood pressure medications that can reduce spasm to specific procedures aimed to reduce the spasm of the vessels induced by the sympathetic nervous system, there is so much that I as a vascular surgeon can do to help patients with Raynaud’s Syndrome. If you think that you might suffer from Raynaud’s Syndrome, please do not hesitate to call our office on 408-376-3626 to schedule an appointment. We Can Help!
Dr. Ignatius H. Lau
Vascular Surgeon
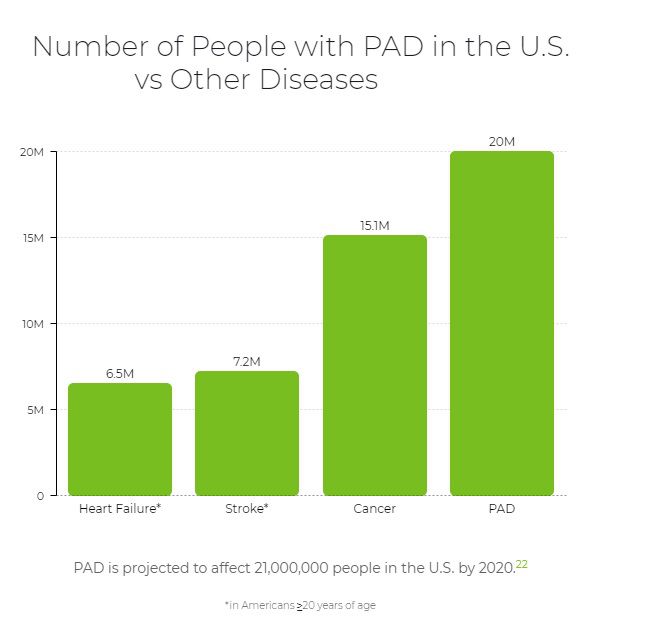
Dr. Ignatius Lau grew up in Portland, Oregon. He attended the University of Washington in Seattle for college and Stony Brook University in Long Island for medical school. He then went on to train in vascular surgery at Mount Sinai Hospital in New York City. During his time in New York, he performed over 1600 cases involving aortic, peripheral, venous, and carotid surgery. He has a special interest in limb salvage and treating patients with peripheral arterial disease and has extensive training and experience in treating the full spectrum of vascular diseases. Dr Lau was also very active in medical research during his training, ultimately finishing with twelve peer reviewed manuscripts. During his training in New York, he met his wife, Lisa, who is a practicing endodontist. Together they love to hike, try new restaurants, and travel.