In part one- and two of our four-part series on “Why do my feet hurt at night”, I discussed Venous disease and Raynaud’s Syndrome. In today’s discussion I want to focus on an even more common reason for why patients may suffer from leg pain at night: Peripheral arterial disease (otherwise known as PAD.)
As we’ve discussed in our earlier blogs, there are two kinds of blood vessels: Arteries and veins.
- Arteries bring blood from the heart to the foot and toes under high pressure while
- Veins bring the blood back from the foot to the heart under low pressure.
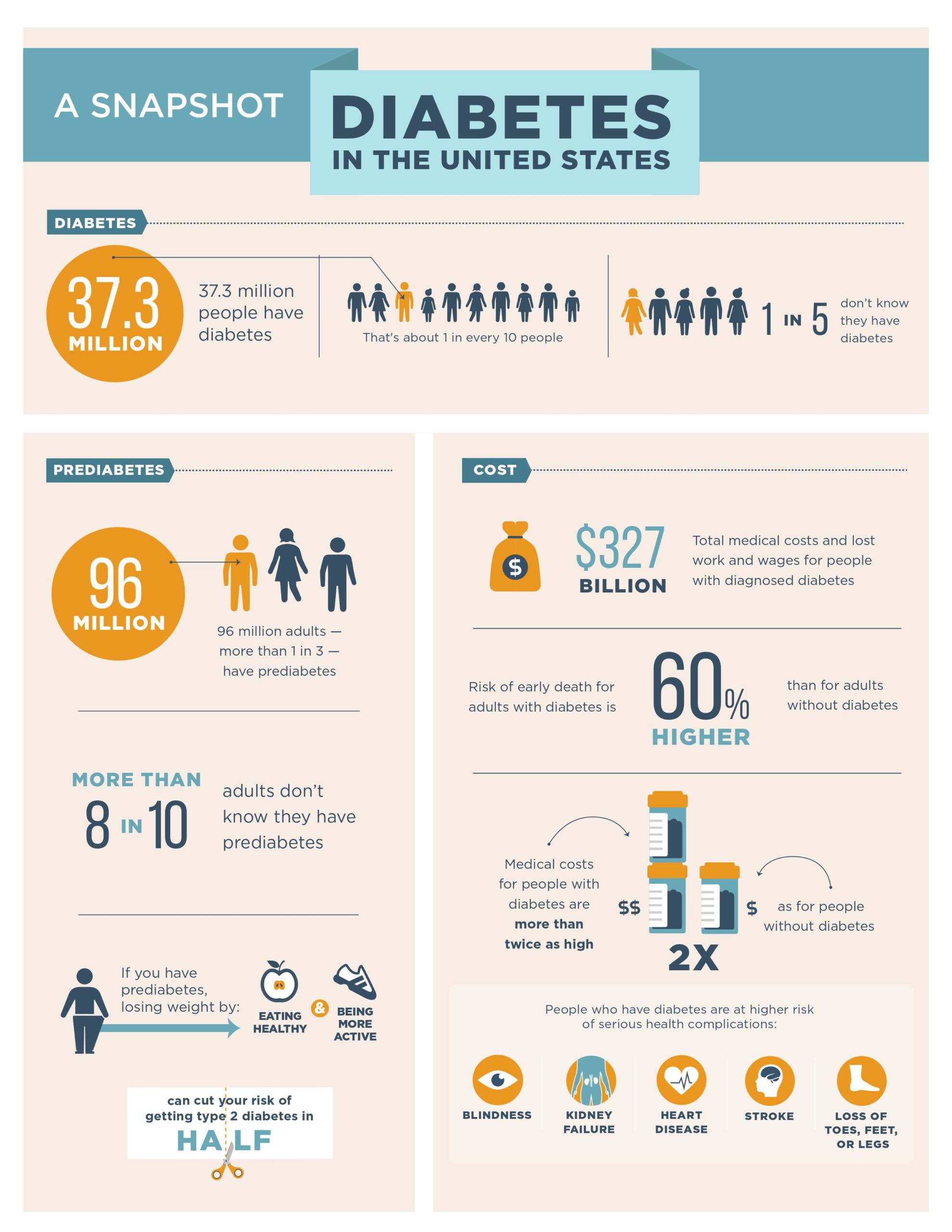
Over the course of anyone’s lifetime, blockages may build up in the arteries between the heart and the feet, especially in the pelvis and the legs. Risk factors that increase the risk of formation of these blockages include:
- Obesity
- High blood pressure
- High cholesterol
- Diabetes
- History of smoking tobacco.
As you may imagine, the tissue within the foot needs a certain amount of blood to supply the nutrients and oxygen necessary to keep the cells within the foot living. Though a single, short segment blockage of the arteries in the leg may not result in any problems, multiple blockages from the pelvis to the foot may can make it difficult or even impossible for the cells within the foot to survive this lack of nutrients and oxygen.
What Does PAD Feel Like?
Typically, patients notice a gradual onset of pain in the forefoot and toes over the course of a few weeks to months. As their blockages worsen, their pain becomes more severe. Pain from PAD occurs in the forefoot and toes because those parts of the body are the furthest away from the heart and thus any blockage along the way from the heart to the toes can contribute to the lack of blood flow. One classic symptom of PAD pain is a burning, tingling, or numb sensation that can be partially relieved by hanging your foot off the bed or a chair. In this position with the foot hanging down, gravity assists the flow of blood to the foot and toes and relieves the pain. Typically, patients complain that when they lay flat at night, the pain in the forefoot and toes or just the foot in general will wake them up. I always specifically ask patients if they are woken up at night by the pain. If they are woken up by the pain, then I know the PAD must be very severe.
In some patients, the lack of blood flow is so diminished that there is also the development of ulcers, or defects in the skin with exposure of underlying fatty tissue, bone, and muscle or gangrene, the death of the tissue itself.
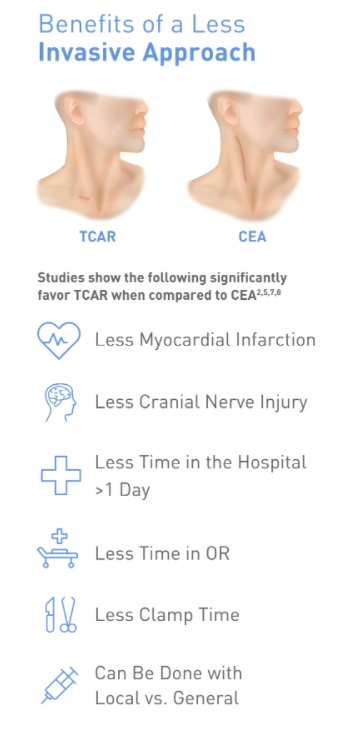
Even though PAD is a very severe and life limiting disease, specially trained vascular surgeons have many tools to combat it! We can do a minimally invasive procedure called an angiogram that I described in an earlier blog post that you can access here! Essentially, I access the diseased blood vessel with a needle and through that needle use contrast and x-ray to see where the blockages are. Then, using balloons, stents, or self-expanding metal tubes, it is possible to re-open the blockages to re-establish blood flow to the impacted area. For severe blockages, I also use a device called atherectomy that allows me to cut through and to remove the plaque responsible for blocking this vessel. The procedure on average takes 1.5 to 2.5 hours and most patients can go home the same day.
Does foot pain wake you up at night? If you are experiencing pain in your foot or toes, please do not hesitate to contact my office at 408-376-3626 to schedule a clinic appointment today!
We Can Help!
Dr. Ignatius H. Lau
Vascular Surgeon
Dr. Ignatius Lau grew up in Portland, Oregon. He attended the University of Washington in Seattle for college and Stony Brook University in Long Island for medical school. He then went on to train in vascular surgery at Mount Sinai Hospital in New York City. During his time in New York, he performed over 1600 cases involving aortic, peripheral, venous, and carotid surgery. He has a special interest in limb salvage and treating patients with peripheral arterial disease and has extensive training and experience in treating the full spectrum of vascular diseases. Dr Lau was also very active in medical research during his training, ultimately finishing with twelve peer reviewed manuscripts. During his training in New York he met his wife, Lisa, who is a practicing endodontist. Together they love to hike, try new restaurants, and travel.