Over the next few weeks, I want to discuss the medications that vascular surgeons may prescribe. These medications include anticoagulants, antiplatelets, statins, and other miscellaneous agents. This week I will discuss anticoagulants!
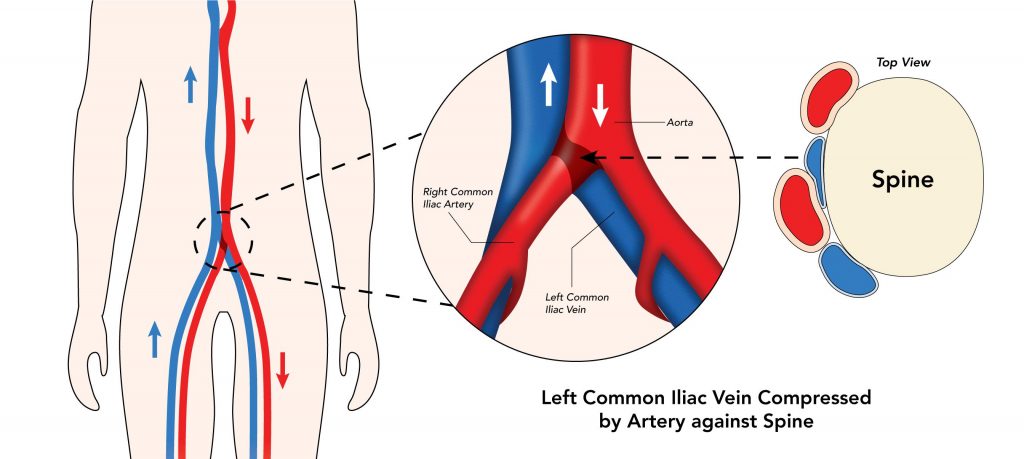
Anticoagulation refers to agents that STOP the clotting of blood. The clotting of blood starts with what is known as the coagulation cascade. The cascade refers to a series of consecutive events each involving special proteins that are needed to occur for blood to form a clot. Different anticoagulants block specific parts of the cascade. The main reason we usually see patients with anticoagulants are for hypercoagulable states, certain heart arrhythmias like atrial fibrillation, and deep vein thromboses otherwise known as blood clots. Hypercoagulable states are specific genetically inherited disorders that result in the blood being more likely to clot. Atrial fibrillation and other arrhythmias can cause blood clots to form in the heart.
Anticoagulant agents are given to prevent the formation of clots in the heart that can then break off and go to the brain, hands, feet, kidneys, or any other part of the body and cause problems.
Deep vein thrombosis or blood clots mandate the prescription of anticoagulant therapy to ensure that more blood clot does not form.
Anticoagulants can be broken up by many different classification schemes. For the purposes of this blog, I will limit our discussion here to agents that are appropriate for the OUTPATIENT (Outside of the hospital) setting. Please speak with you private physician to answer any additional questions you may have regarding Anticoagulation medication of feel free to reach out to me directions for more information on how anticoagulation is used. Anticoagulation agents that are used during hospitalization or in the IN-PATIENT setting in patients are outside the scope of this article.
Up until the 2010’s the mainstay of anticoagulation therapy was with a drug called warfarin (Trade name: Coumadin). Warfarin, though effective, requires the weekly or biweekly measurement of a specific lab for the blood called the prothrombin time. The active monitoring of the prothrombin time facilitates modulation of dosing to always allow for safe levels of effective therapeutic anticoagulation. Since the beginning of the 21st century new agents have come to market that require only taking one or two pills a day. They include Xarelto or Rivaroxaban and Eliquis or apixaban.
If you have a question about how your medications may be affecting your vascular disease, please do not hesitate to call and schedule an appointment today!
South Bay Vascular Center and Vein Institute is Silicon Valley’s largest and most trusted Vascular Surgery practice. Serving South Bay communities for over 26 years, Dr Kokinos and her Colleague, Dr Ignatius Lau are the region’s foremost experts in advanced vascular care and provide innovative care for patients suffering from circulation relation problems. At South Bay Vascular Center and Vein Institute our job is to understand the “Why” so that you have real solutions to living a healthy life. Call us today at 408-376-3626 or visit our website at www.southbayvascular.com to learn about what makes us the most referred to vascular surgery clinic in Silicon Valley.