One of the many questions I receive as a vascular surgeon is why do my feet hurt at night? Though this question may seem simple, every person is different. Before I can provide you with “real” solutions to what’s causing this pain and what can be done to stop it, I need to evaluate multiple factors to understand “Why” this pain exists. Over the next few weeks, I am going to explore the most common reasons for foot pain at night and why people can have pain in their feet at night caused by venous disease.
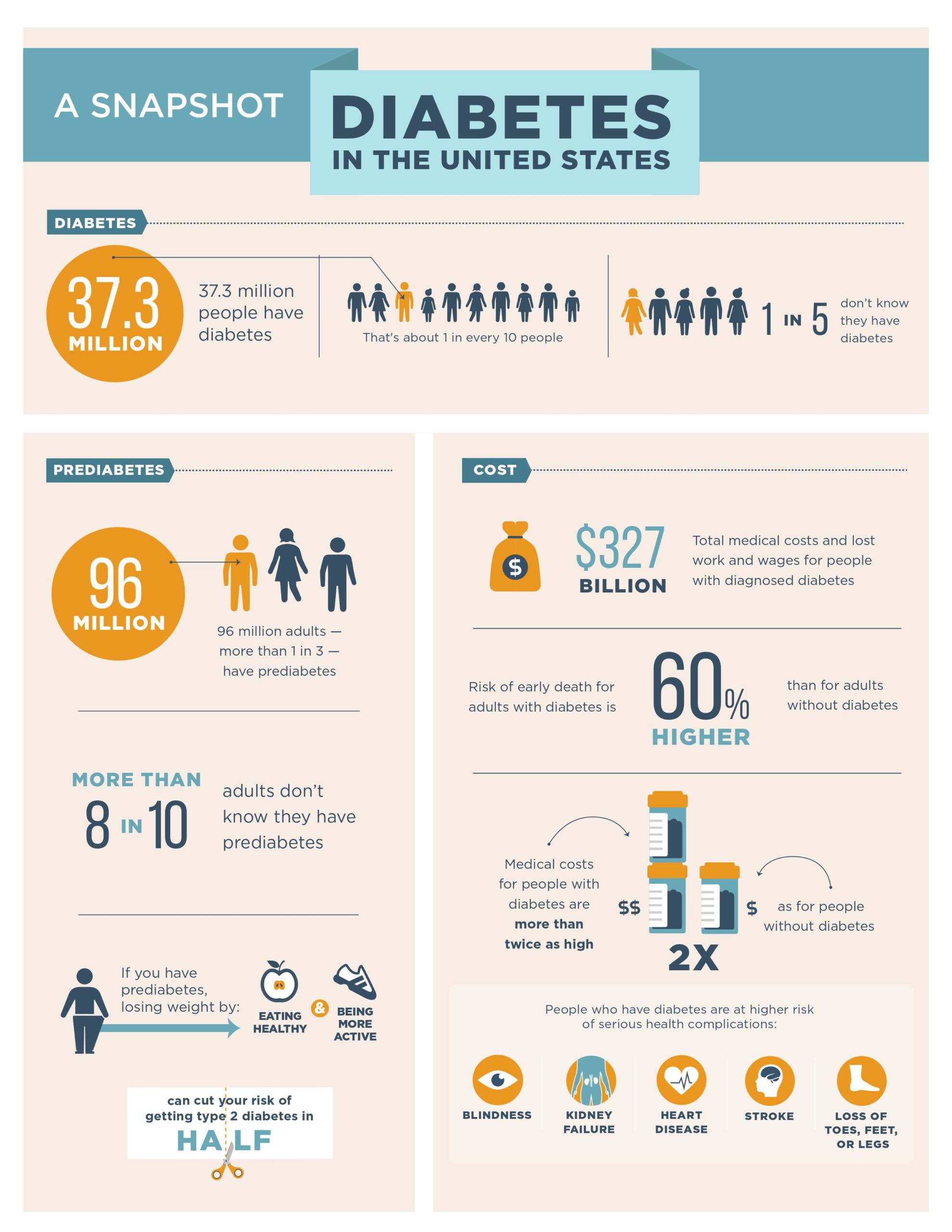
For the majority of patients Raynaud’s syndrome, Arterial disease, and Diabetic foot disease explain most of the reasons why people experience pain in their feet at night. Though pain from problems with bones and muscle can play a role, pain due to these causes usually worsens during the day and with use, not when a patient is resting or lying flat.
In part one of this four-part series, I am going to discuss pain at night caused by VENOUS DISEASE.
Let’s start with a refresher on our bodies “plumbing” (Specifically, how does blood circulate around my body.)
- Veins are blood vessels that bring blood BACK from the feet to the heart.
- Arteries on the other hand are the blood vessels that bring blood FROM the heart to the feet.
Veins have specialized structures called one-way valves that allow blood to go up towards the heart but not back down towards the feet. As we age, veins become dilated (start to leak) because the valves no longer seal properly. These leaky valves allow blood to fall back towards one’s feet which results in an increase in pressure within the veins at the ankle and just above the legs. Gravity tugs on the blood in our veins bringing it down to our feet which causes this increase in pressure
Interestingly, because of the curve that the veins take at the level of the ankle to enter the foot, the increase in pressure is not transmitted directly to the foot and toes. The increase in venous pressure at the ankle typically results in
- Varicose veins,
- Swelling,
- Dark skin discoloration from the leaking of red blood cells into the skin, and, in the worst cases
- Ulceration.
Even without ulceration, however, the pain related to swelling and discoloration can be very severe.
People during their normal daily lives spend most of their days either standing or sitting. Because of this, during the day gravity works in both positions to facilitate the pooling of blood around one’s ankles. When patients come to me with pain in their feet, I always ask specifically if the pain is localized in the calves and ankles. When pain is localized to the calves and ankles, I confirm a venous etiology by performing a physical exam and finding varicose veins, swelling, dark skin discoloration and/or ulcers between the ankle and the knee.
Pain that is reported in the foot and/or toes without the physical exam findings of varicose veins, swelling, dark skin discoloration, and/or ulcers between the ankle and the knee is NOT likely to be from a venous cause! Though vein problems may sound or seem like a rare disease for those who have never had venous disease, patients with vein problems are one of the most common consults I see as a vascular surgeon. Does foot pain wake you up at night? If you have any of the symptoms or appearance of the leg that I described above, please do not hesitate to call our office on 408-376-3626 to schedule an appointment.
One Final Note:
Though causes from the bones and muscles can play a role, foot pain that worsens at night is rarely due to these causes. Often pain related to problems with bones and muscles worsen during the day and with use, not when any given patient is resting or lying flat.
Clues that can guide me as a vascular surgeon to the cause include throbbing and aching pain versus numbness and tingling associated with tenderness or pain located in the toes versus pain located in the ankle or just above the ankle in the leg.
Dr. Ignatius H. Lau
Vascular Surgeon
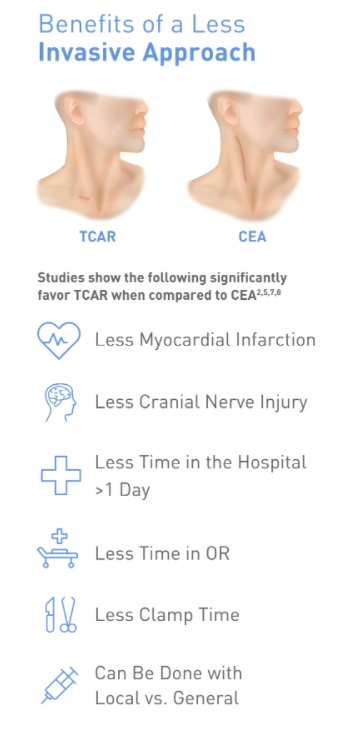
Dr. Ignatius Lau grew up in Portland, Oregon. He attended the University of Washington in Seattle for college and Stony Brook University in Long Island for medical school. He then went on to train in vascular surgery at Mount Sinai Hospital in New York City. During his time in New York, he performed over 1600 cases involving aortic, peripheral, venous, and carotid surgery. He has a special interest in limb salvage and treating patients with peripheral arterial disease and has extensive training and experience in treating the full spectrum of vascular diseases. Dr Lau was also very active in medical research during his training, ultimately finishing with twelve peer reviewed manuscripts. During his training in New York he met his wife, Lisa, who is a practicing endodontist. Together they love to hike, try new restaurants, and travel.