Do you Suffer From Iliac Vein Compression?
To answer that question, take a few seconds to consider the following:
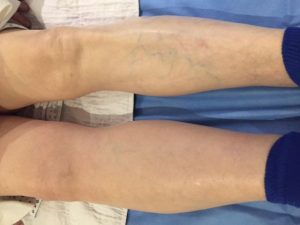
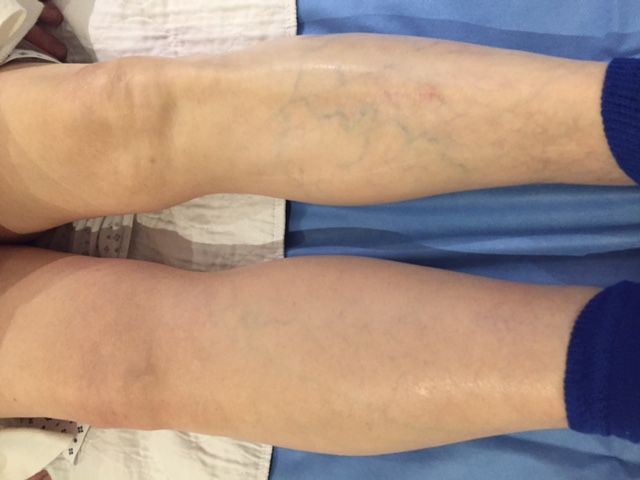
- Are your legs swollen? Is your left leg larger than your right?
- Is it harder to slip one shoe on in the morning than the other?
- Have you had cosmetic or other surgical procedure done and not gotten the outcome you wanted?
- Are you a cancer patient undergoing treatment or procedures?
- Have you ever suffered from a blood clot or (DVT) in your leg
- Do you visit a wound care clinic with little to no success?
If you’ve answered yes to any of these questions, you MAY be suffering from a well known, but previously difficult to diagnose problem called May-Thurner’s Syndrome.
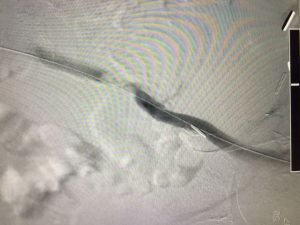
May Thurner’s Syndrome, also known as iliac Vein Compression, is a condition where the main artery supplying blood to the leg pushes down or compresses the main vein taking blood back to your heart. In the illustration below you can see in the far right graphic a “representation” of this compression. One way to help think of what happens when a patient suffers from iliac vein compressions is to consider what happens when a car tire partially runs over a garden hose in your driveway.
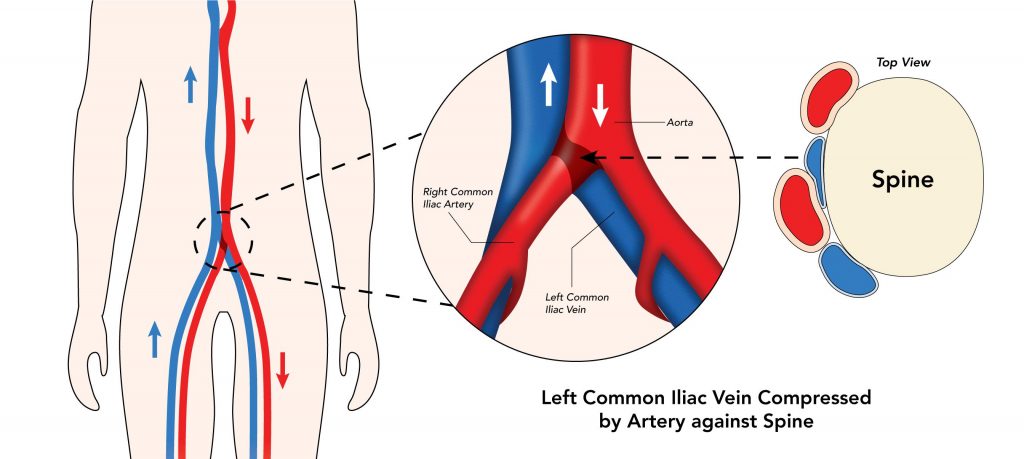
If the hose was “on” when you drove over it, water will continue to come out of the hose end but the flow rate will decrease. In a similiar way, blood returning to your heart will continue to flow if you have developed iliac vein compression, but the rate at which it returns is slowed down, resulting in a pooling of blood (i.e. swelling) in your leg.
Chronic pain and swelling in one leg (especially the left side) may be caused by Iliac Vein Compression. This is a little-known but fairly common condition that can greatly impact your quality of life—and may lead to more serious complications. In fact, studies have shown that in a full 30% of ALL people, the left iliac vein can be significantly compressed by the right iliac artery resulting in some kind of leg symptom….aching, heaviness, and most commonly, swelling or non-healing of wounds in the leg veins.
Swollen legs ARE NOT a normal part of aging or weight gain. And it’s not something you have to “just live with.”
Leg swelling is a special area of interest of Dr. Polly Kokinos, and she has been active in doing clinical research to find better ways to diagnose and to treat this condition. To diagnose and to treat this condition and the potentially deadly side effects caused by it (Blood Clots or Deep Venous Thrombosis) Dr. Kokinos has assembled a highly skilled team of vascular ultrasonographer’s who have developed a specialized screening protocol to evaluate for Iliac Vein Compression. Using state of the art ultrasonic imaging technology Dr. Kokinos’ Registered Vascular Ultrasonographer’s use this new protocol to scan up into the abdomen of their patients to examine the physics of the blood flow in this area. If a compression is identified during this ultrasound exam, Dr. Kokinos is able to further verify and treat this problem using a super specialized device called IVUS (Intra-vascular ultrasound) where she can insert a miniuture camera into the actual vein to determine the length of the compression after which she can place a stent to “re-open” this compressed vessel to re-establish normal blood flow.
To date, Dr. Kokinos has successfully performed over 200 of these iliac vein stent procedures in her state of the art out-patient angiography suite. She has lectured extensively at major vascular surgery meetings on her approach and success helping patients reduce leg swelling, increase the rate of wound healing and return to a normal way of living and is seen by her peers as an expert in this technique.
If you are currently experiencing a swollen leg, have a non healing leg, foot,or ankle wounds or have ever suffered a blood clot (DVT) please contact our office at 408-376-3626 to schedule an appointment.
Don’t suffer from swollen legs or non-healing leg ulcers any longer.
We can help!